Eye Care and Vision Health
Eye structures
The Orbit
Eye socket

Bones
The bone structure that surrounds the eye
- A safety pocket for the eyeball to rest in
- Extra space around holds fat, blood vessels, nerves, muscles, etc.
Eyelid 眼瞼
- The skin covers and protects the eye from injury.
- Blinks keep the eye moist , distribute tears over the front surface (i.e. cornea)
- When your eyelids are closed, they keep the lights out
- Eyelashes protect the surface of the eye
Tears 溢淚
Tears Contains
- Water
- Oil
- Mucus
Babies don’t make tears until they are 4-6 months old.
Mothers should bring their babies for a check-up if they notice their babies do not produce tears after 6 months of age
Eyelid 眼瞼
Secretes oils and mucous into tears.
Extra-ocular Muscles
6 muscles are used by the eyeball to control eye movement.

- Normal eye movement moves in synchrony
- E.g. Right and left eyes move down together at the same rate
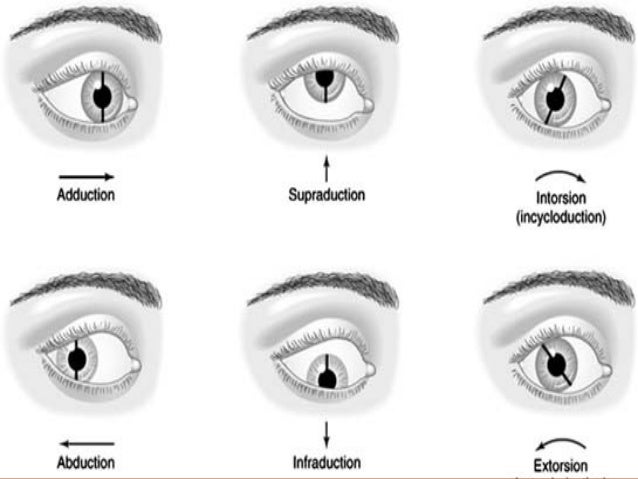
Eye Movements
- Adduction (Move Rightwards)
- Abduction (Move Leftwards)
- Supraduction (Move Upwards)
- Infraduction (Move Downwards)
- Intorsion / Incycloduction (Rotate Inwards)
- Extorsion / Excycloduction (Rotate Outwards)
Eye Positions
- Esotropia
- Exotropia
- Hypertropia
- Hypotropia

The Eyeball
Conjunctiva 結膜 & Sclera 鞏膜
Conjunctiva is an invisible layer covering the front part of the eye, lining the eyelid.
Purposes:
- Slippery surface helps the eyelid to glide smoothly over the eye during blinking
- Protects and nourishes the eye
The structure underneath is called the Sclera (the white opaque portion), covering around the back of the eye
Problems in conjunctiva
Pterygium (翼狀贅片)
- Elastotic degeneration of collagen and fibrovascular proliferation
Pingueculae (結膜黃斑)
- Degradation of sub- epithelial collagen fibres.
Cornea 角膜
Major refractive component
- Transparent: to allow light to enter our eyes (where light first enters)
- Avascular: No blood vessels
Layers of the Cornea:
- Epithelium
- Bowman’s Membrane
- Stroma
- Descemet’s Membrane
- Endothelium
Iris 虹膜
The colour part of the eye
- Thin structure with a central opening
- functions like the diaphragm of a camera
- Pattern of iris is unique to each individual, just like fingerprint
You can wear an Artificial Iris, makes your iris looks more colored.
Pupil 瞳孔
The central opening of the Iris
- Can change size to control the amount of light entering our eyes
- Size of pupil: 1 to 8mm
- Smaller under bright conditions but larger under dark conditions
- Size is also affected by a person’s mood (i.e., pain, pleasure, fear)
- The pupil size reduces/enlarges as one grows old

Controlled by 2 muscles of the Iris
- Sphincter muscle (pupil constriction)
- Dilator muscle (pupil dilation)
Pupil Abnormalities
- Unequal or dilated and unreactive - suspect brain herniation
- Unilateral or bilateral pupils - asymmetric pupils differ > 1mm
- Dilated pupils - dilation more than or equal to 4mm
- Fixed pupils - fixed pupil less than 1mm change in response to bright light

Lens 晶體
Locate behind the Iris.
- An Important component to focus incoming light on the retina.
- lens becomes denser and less flexible with age
- held by ciliary muscles and ligaments
- Surrounding muscles are flexible to change the shape of the lens which allows our eyes to see objects at different distance.
- Accommodation: The ability of the eyes to clearly focus on objects at different distances.
- After 40 yrs old, our accommodation power decrease gradually.
Cataract
A Cloding of the lens of the eye which leads to a decrease in vision.
- Stellate Cataract
- Anterior Polar Cataract
- Cotical Cataract
- Posterior Subcapsular Cataract
- Nuclear Cataract
Aqueous Humor 眼房水
The clear watery fluid that fills the front empty space of the eye
- Provides nutrients to the front and back surfaces: cornea and lens
- Constantly produced and drained to maintain normal eye pressure
Vitreous Humor 玻璃體
A transparent, gel-like substance that keeps the eyeball structures in place
- Very viscous and does not regenerate
- Made of mostly water and takes up 2/3 of the eye’s volume and weight

Floaters
- Due to part of the eye that is loosing its viscosity and degenerating
Intraocular pressure (IOP)
the fluid pressure inside the eye
Glaucoma is a group of eye conditions that damage the optic nerve, the health of which is vital for good vision. This damage is often caused by an abnormally high pressure in your eye.
Retina 視網膜
A semi-transparent layer that covers the back of an eye.
- Made up of 10 layers of specialized cells, such as nerve cells and photoreceptors.
- Receiving and transferring light signals to the brain.
Macula and Fovea
- A point on the retina responsible for your central vision
- The FOVEA is the center point of the macula responsible for the clearest vision you perceive
Optic Nerve
A continuation of the retinal layer towards the brain
Common vision problems
Refractive Errors (屈光不正)
Myopia (nearsightedness/ short-sighted/近視)
The most common refractive error in the Asia-pacific regions (70-90%).
The 7th leading cause of legal blindness in the United States and the 4th leading cause of blindness in Hong Kong.
Symptom:
- Blurry vision
- Cannot see distance objects clearly
- or high myope, cannot even clearly identify objects at near.
Caused by:
- Abnormal Eyeshape - Slightly elongated eyeball
- light is focused just in front of retina instead of on it


Pinhole effect allows you to see things easier.
Hyperopia (farsightedness/ long-sighted/遠視)
Symptom:
- Have problems focusing on near objects
- Eye discomfort
- Distance vision usually unaffected
- Decreased near vision (high hyperopia)
- Associated with certain types of eye turn or a lazy eye
Caused by:
- light is focused just behind retina instead of on it

Pinhole effect allows you to see things easier.
Astigmatism (散光)
Symptom:
- Blurred vision
- Decreased vision at both far and near
- Eye discomfort
Presbyopia (老花)
Symptom:
- Headaches after reading for a long time
- Needs bright lighting to read better
- Trouble focusing on words up close
- Stretches arms to put reading materials at a long enough distance in order to make the prints readable
Caused by:
- Aging process
Corrections for Refractive Errors
Optical Correction
- Spectacle Glasses
- Contact Lenses
Refractive Surgery
- Laser assisted in-situ keratomileusis (LASIK)
- try to correct the cornea or lens shape back to a normal power in order to focus on objects without the need of glasses
Consequences of non-correction
Lazy Eye (Amblyopia)
- Might happen if children are not given a proper glasses prescription before their critical developmental period (before 8 years old)
- Once Lazy Eye developed, vision could NOT be improved with ophthalmic aids or surgery.
- Permanent loss of partly vision
Basic Tests in Vision Screenings
Visual Acuity 視力
Visual Acuity (視力) - Ability of visual system (eye + brain) to resolve spatial detail
Purpose of Visual Acuity Measurement
- To quantify the habitual visual performance
- How well a person sees normally
- To identify ocular abnormalities
- Refractive errors
- Diseases (structural & functional)
- To assess a person’s ability to meet certain task requirement
- Driver, pilot, vessel operator
Construction of letter chart
-
Hard for patients to describe to you what they see
-
Fonttype: Optotypes
- Tumbling E
- Landolt ring
- Alphabet
- Number
- HOTV Test
- LEA symbols
Snellen Letter Chart
Developed by a Dutch ophthalmologist, Dr Herman Snellen in 1862
Modern Snellen Letter Chart
Letter size = distance recognized by a normal person
Snellen’s Notation for Visual Acuity
Numerator : Testing distance
Denominator : Font size of the smallest letter the patient seen
Interpretation of Visual Acuity
Snellen Fraction:
Numerator : Xm (Patient can recognizes the letter at Xm)
Denominator : 18m (Nomal person average value)
Visual Acuity Assessment
Presentation of Visual Acuity Charts
- Testing distance = 6m (Britain) / 20 feet (USA)
- Height level = 3m/10ft (Eve level)
Clinical Procedures
- Test the right eye first
- Instruct the participant to cover the left eye and read the chart using the right eye
- Read the first/last symbol in each line from top to bottom
- Proceed to following line until the participant misidentifies a symbol
- Go back to previous line and ask the participant to read all the symbols on that line
- Proceed to following line if the participant can read more than half of the symbols on that line
- The visual acuity level is the last line in which more than half of the letter in that line are correctly recognized
- Cover the right eye and repeat the above steps with left eye
Colour Vision 顏色色覺
Why screen for colour vision?
- Eye diseases
- E.g Optic neuritis, age-related macular degeneration
- Some drugs may cause colour vison deficiencies
- E.g. Phenelzine (Antidepressant), Ethambutol (Antitubercular agent), Hydroxychloroquine (Antirheumatic and antimalarial drug)
- Occupational requirements
- Better to know earlier so can better plan their career path
- Students with severe colour vision defect may be mislabelled as learning disabled
Common Color Vision Tests
| Test | Screening | Congenital Red-Green deficiency | Acquired color deficiency | Color deficiency classification | Severity determination | Pediatric version | Time |
|---|---|---|---|---|---|---|---|
| HRR 4th Edition | √ | √ | √ | √ | Mild/Medium/Strong | √ | Very fast |
| Color Vision Testing Made Easy | √ | √ | X | X | x | √ | Very fast |
| Ishihara – 24 plates version | √ | √ | X | √ | Mild/Strong | Separate | Quick |
| City University (3rd edition) | √ | √ | √ | √ | X | X | Moderate |
| Farnsworth D15 | X | √ | √ | √ | Medium/Strong | X | Slow |
| Lanthony Desaturated 15 | X | √ | √ | √ | Mild only | X | Very slow |
Ishihara
- Only for congenital red- green colour vision defect
- Daylight illumination
- Available in 38-, 24-, and 16- plate versions (24- and 16- most common)
Pros:
- Readily available & easy to conduct
- Accurate
- Inexpensive
Cons:
- Can’t detect Blue-Yellow defect
- Number of errors NOT intended to be an index of severity
Clinical Procedures:
- Participant can wear their spectacle correction
- Chart at 75 cm (perpendicular to line of sight)
- Usually test binocularly (in children)
- Number (Literate) vs. line tracing (illiterate)
- Do NOT allow participant to touch the plates
- Viewing time: 3 seconds / plate (Number), 10 seconds/plate (line tracing)
- Record score as number of plates correct
H.R.R. Pseudoisochromatic Plates Test:
-
Working distance = ~75 cm (30 inches)
-
Viewing time: ~ 3 secs/plate
-
Test monocularly
-
Pages 1-4: Demonstration
-
Pages 5-10: Screening
-
Page 11-24: Diagnosis
-
For each plate, ask:
- – Number: How many symbols do you see?
- – Name: What are they?
- – Location: Where are they?
-
Participant can get the score of that plate if they can correctly answer the above three questions
What to do after colour vision testing?
Follow up:
– Indication of colour deficiency
– Detailed diagnostic colour tests
– Macular and optic nerve functions
Stereopsis (3D) 立體感
- Ability to judge depth by coordinating visual signals from both eyes
- Advantage : judge distance with great precision
- Important for eye-hand coordination
Clinical Tests for Stereopsis
- Stereo Smile 3 Test
- Random dot Stereo Acuity Test with Lea Symobols
Preschool Assessment of STEREOPSIS with a Smile (PASS) – Clinical Procedures
- Hold the test card 40 cm away from participant
- Ask the participant to wear the polaroid glasses (on top of habitual glasses, if any)
- Put the Card A (DEMO card) and blank card side by side in front of the participant and ask them to identify the card with “Smiley Face” on it
- Shuffle the cards and change the card position in a random manner
- Repeat step 3-4 for a maximum of 5 times.
- Proceed to next level if the participant can identify the “Smiley face” for 4 out of 5 times
- Record last card with 4 out of 5 times Correct
Random Dot Stereo Acuity with Lea Symbols – Clinical Procedures
- Instruct the participant to wear the polaroid glasses over their habitual glasses (if any)
- Put the booklet at 40 cm in front of patient
- Ask the participant to identify the box which does not contain any figure in each section (A, B, C, D). Do not allow any head movement during the test.
- Proceed to box number 1
- Ask the participant to identify the popping circle in each section. Encourage the participant to make a guess if they cannot identify one
- Proceed to next box and repeat Step 5 until the participant misidentifies the popping circle
- Record the corresponding stereoacuity of the last box in which the participant is able to identify the popping circle
Cover/Uncover Testing 遮蓋測試
Types and Characteristics of Ocular Deviation
-
Heterotropia(or Strabismus/squint) 斜視
- Manifested ocular deviation
- Cannot be controlled by fusion 不能通過融像被控制
-
Heterophoria 隱性斜視
- Latent ocular deviation
- Usually not noticeable
- Compensated by fusion mechanisms 可以被融像機制 補償
- Revealed with dissociation 於解離中顯露出來
-
Causes of Ocular Deviation
- Congenital: developmental anomalies
- Acquired: due to disease or injury
Detection of Ocular deviation
Cover Test 遮蓋測試
- Unilateral cover test 單側遮蓋測試
- Is there an eye turn/manifest deviation/tropia?
- Alternating cover test 交替遮蓋測試
- Is there any latent eye deviation?
Motility (Extra- ocular muscle: The H Test)
- Eye muscles are hidden in the orbit
- Structural assessment is not feasible
- The muscles are innervated by three of the cranial nerves
- Functional assessment
- Contraction of EOMs leads to eye movements
- Compare the eye movements with expected norms
- Under- or over- action is classified as abnormal
Confrontation
Purpose of Visual Field Screening
- Test for peripheral vision
- Detection of retinal and neurological (visual pathways) diseases
Confrontation is Performed face to face (Gross visual field test).
-
Finger-counting
-
Small target counting
Amsler Grid 阿姆斯勒方格
- Central field screening
- Design for detecting macular lesions
- Consists of 7 charts of varying patterns which subtends 20 degree horizontally and 20 degree vertically
Clinical Procedures
- Instruct participant wearing reading glasses (no progressive lenses), if any, and cover the non-tested eye.
- Put the Amsler grid at a working distance of 28-30cm
- Instruct the participant to fixate at the central white dot and identify any lines that are distorted, faint, missing or blurred
- Note and record the location and number of boxes involved
Can be used to test with Age-related macular degeneration (老年黃斑病變)
Pupil Testing
Purpose of Pupil Testing
- provides information about the integrity and function of iris, optic nerve and brain
Clinical Procedures
- Dim the room light.
- Take off the participant’s glasses and instruct the patient to look at distant target.
- Compare the pupil size and shape (round and equal in size). • Check for any anisocoria (difference in pupil size between eyes > 1mm)
- Shine the penlight close to line of sight of right eye. The right eye pupil constricts. Observe the pupil response of right eye.
- Remove the penlight and observe the dilation of the right eye pupil.
- Shine the penlight to the line of sight of right eye but observe the left eye (contralateral) pupil response if it constricts equally the same as the right eye.
- Repeat step 4-6 on the left eye pupil.
- Shine the eyes alternatively by maintaining a steady light for 3-5 sec in front on each pupil
- Observe the pupil reactions
- Repeat step 8 and 9 for 3 cycles
Auto-refraction 電腦驗光度數
Tentative findings ONLY; can’t be used for prescription
Clinical Procedures
- Disinfect forehead and chin rest
- Seat the participant in front of the instrument
- Instruct the participant to take off the glasses and put his/her head on headrest and chin on the chinrest
- Align the eye level by adjusting the level of the chinrest
- Instruct the participant to look at the fixation target
- Move the instrument forward or backward from the participant’s eye using the joystick to take a sharp focus
- Take 3 measurements
- Print the result
Intraocular Pressure
Non-Contact Tonometry (NCT)
- Tonometry: Measurement of Intra-ocular pressure (IOP) (eye pressure)
- Applanation class of tonometry
- A puff of air to flatten a circular area of cornea ~3 mm in diammeter
- Advantages
- Fast and easy
- No anesthetic is required
- Useful for patients who are allergic to topical anesthetic
- Disadvantage
- Uncomfortable
- Referral criteria
- < 6mmHg
- >21mmHg
- >3mmHg difference between eyes
Limitation of glaucoma (青光眼) screening by tonometry

Clinical Procedures
- Disinfect forehead and chin rest
- Seat the participant in front of the instrument
- Instruct the participant to take off the glasses and then put his/her head on headrest and chin on the chinrest
- Align the eye level by adjusting the level of the chinrest
- Instruct participant to close his/her eyes
- Move the instrument slowly towards the participant’s eye using the joystick, while pressing the safety button along- side the instrument
- Release the safety button when the air nozzle is 8-10 mm away from the participant’s eye
- Gently move the instrument forward to make sure that the instrument will not move beyond the locked position
- Take 3 measurements from each eye
- Print the results
Latest technology
- iCare tonometer
- Rebound technology
- A very light and slow moving probe
- Momentary contact with cornea
- No anesthetics is required
- Hand held
